 The first doses of a Covid-19 vaccine were administered on Dec 14, 2020, about a year after the disease was first detected. Tested, FDA-approved for emergency use, rapidly manufactured and safely delivered at sub-freezing temperatures, this was, by any measure, the fastest pathway to vaccination in human history.
The first doses of a Covid-19 vaccine were administered on Dec 14, 2020, about a year after the disease was first detected. Tested, FDA-approved for emergency use, rapidly manufactured and safely delivered at sub-freezing temperatures, this was, by any measure, the fastest pathway to vaccination in human history.
One of the latest examples of development from scratch was the mumps vaccine in the 1960s. It took four years to complete and release, which at the time was considered extraordinarily quick. However, until recently, developing a vaccine required approximately 10 years and $500 million. How many lives could be saved if this timeline could be significantly accelerated from now on?
It is generally known that the pharmaceutical industry undergoes scrutiny when developing new treatments—testing protocols and the FDA-approval process—all of which were highly compressed for Covid-19 vaccines. But up until this current situation, part of the industry use to rely on outdated supply chains, older processing equipment and manual methods. These existing technologies and routines have been all major contributors to the length of the average vaccine’s journey to market.
Just as the pandemic has forced countless of industries to speed up their digital transformations, so, too, will it prove a tipping point for biopharma companies.
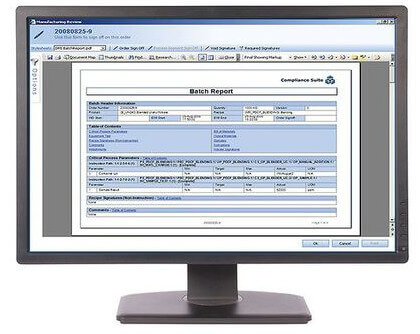 Accelerating vaccine development requires unprecedented flexibility in managing data. With increasing integration between product lifecycle management systems and software—like distributed control systems (DCS) and manufacturing execution systems (MES)—data, recipes, and processes can be digitally altered, shared, and used to scale across the lifecycle.
Accelerating vaccine development requires unprecedented flexibility in managing data. With increasing integration between product lifecycle management systems and software—like distributed control systems (DCS) and manufacturing execution systems (MES)—data, recipes, and processes can be digitally altered, shared, and used to scale across the lifecycle.
Data management must work together with manufacturing, and that’s where actual equipment and instrumentation comes into the picture. Today’s versatile transmitters can interface with multiple sensors or multiple kinds of sensors, including pH, ORP, and conductivity. With internal diagnostic functions, they can detect a problem developing and warn operators before a batch is lost.
“Digital transformation technology has been a key enabler to the development and delivery of Covid-19 vaccines at such a rapid speed,” says Jim Nyquist, Chairman of Systems and Software at Emerson, a CESMII [Smart Manufacturing Institute] member. “In a few years, today’s record-breaking digitalized manufacturing will have become the norm for delivering life-saving therapies to patients.”
Indeed, such technologies are challenging the idea that the various stages of vaccine development need to occur sequentially at all. “Digital transformation technologies shift the typically serial process of a drug’s life cycle into compact, parallel processes leveraging digital automation,” Nyquist says. “This can turn years into months and months into days.”
Like the Covid-19 shots, most vaccines need to be kept cold to avoid spoilage. A broken link in the cold chain means wasted time and money for drug companies and further delay for patients. Cold chain failures cost the pharma industry $35 billion per year, yet many companies continue to rely on outdated methods to warn of temperature changes. In recent years, monitoring technology has evolved to include highly automated networks of sensors and servers that collect a broad range of data in real-time and send out alerts when fluctuations occur.
Emerson is committed to help the pharmaceutical industry to realize the advantages of these recent developments, through our digital transformation solutions and make the next vaccine development—and even day-to-day production—more efficient, effective, and profitable.
Visit the Life Sciences & Medical section on Emerson.com for more on the technologies and solutions to drive performance improvements in vaccine and therapeutics time to market.




